American Heart Month: Keeping a Pulse on Heart Disease

Nearly half of U.S. adults are living with heart disease, but not everyone understands the range of conditions that encompasses. Heart disease is a commonly used term that most frequently refers to coronary artery disease, but also includes conditions like arrhythmias (abnormal heart rhythms), heart failure, heart valve disease, congenital heart disease, aortic disease, and more.
The prevalence of heart disease increases with age. While it only affects 1% of people aged 18 to 44, it jumps to 14% among people aged 65 to 74, and 24% in people 75 and older.
The good news is there are several steps you can take to reduce your risk of developing heart disease as you age. Swapping an ultra-processed snack for a piece of fruit or whole grains is one step toward a more heart-healthy diet. Consistently exercising and not smoking are important prevention methods, too. Each of these preventive steps can help stave off two of the biggest risk factors for heart disease: hypertension (high blood pressure) and high cholesterol.
Perhaps an underrated component of a healthy lifestyle and cardiac health is sleep. The ideal amount of sleep will vary from person to person. However, the American Heart Association recommends seven to nine hours of sleep nightly to improve cardiovascular health.
This Heart Health Awareness Month, here's how you can implement more heart-healthy habits in your everyday life, and advancements in the cardiology field you should know about.
— Christopher Lee, MD, cardiologist and Verywell Health Medical Expert Board member
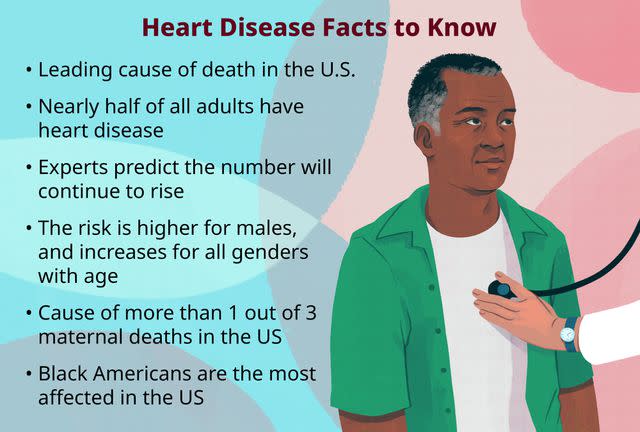
Illustration by Mira Norian for Verywell Health
In the Headlines
Easy Ways to Protect Your Heart
Ask the Expert
For someone who is just beginning to monitor blood pressure and cholesterol levels, is it more important to start with a focus on diet or exercise?
Dr. Lee: Both diet and exercise are important when thinking about controlling your blood pressure and cholesterol levels. But if you are going to start with one, improving your dietary habits plays the most critical role. Dietary plans such as the DASH diet and Mediterranean diet significantly improve blood pressure, cholesterol levels, and weight management. No amount of exercise can compensate for poor dietary habits.
When does high blood pressure warrant medication, and which classes of medication are typically prescribed first?
Dr. Lee: Doctors stage high blood pressure according to the American College of Cardiology and American Heart Association Guidelines from 2017, defining stage I hypertension as a systolic blood pressure ranging from 130-139 mmHg and a diastolic blood pressure of 80-89 mmHg. If you have been diagnosed with hypertension, our initial interventions to improve your blood pressure include weight loss, dietary changes, and increasing your level of physical activity.
If your blood pressure remains elevated, we will consider starting a medication. We also calculate your 10-year risk of cardiac events to help make this decision. Medication therapy is individualized per patient, but some of the more common first-line medications we use include diuretics (such as hydrochlorothiazide or chlorthalidone), ACE inhibitors/ARBs (such as lisinopril or losartan), and calcium channel blockers (such as amlodipine).
Who is a good candidate for a statin, and what do you wish people with high cholesterol knew about statins?
Dr. Lee: Statins are the most commonly used medications to lower cholesterol. However, doctors look at more than just your cholesterol levels to determine whether you are a good candidate for a statin. If you have not previously suffered a cardiac event, we use statins for "primary prevention," or to prevent or delay an initial cardiac event.
We also consider your sex, blood pressure, ethnicity, smoking status, and whether you have been diagnosed with diabetes to determine your risk of having a cardiac event within the next 10 years. If you have an elevated risk, you are a good candidate for starting a statin. If you have previously had a cardiac event, statins are used for "secondary prevention," or to prevent major adverse cardiac events and death.
I think that statins are often unfairly vilified. A significant percentage of patients who may benefit from statins stop their medications due to perceived side effects. Statin-induced side effects are rare, but one of the most commonly mentioned side effects is muscle pain. However, one study showed that when patients were either given a statin, a placebo, or neither, the majority of side effects that developed while patients took a statin also developed among those taking a placebo pill.
What advancements in heart disease treatment are you most excited about from the past year?
Dr. Lee: The use of glucagon-like peptide-1 (GLP-1) receptor agonists (e.g., Wegovy and Ozempic) for both weight loss and cardiovascular health has been an exciting development in the world of cardiology. GLP-1 agonists have traditionally been used in the treatment of diabetes, but more recent data has shown that they can also reduce major adverse cardiovascular events.
Prior trials have established that GLP-1 agonists are most helpful in patients with (or at high risk of) atherosclerotic cardiovascular disease with type 2 diabetes. A recent trial published in the New England Journal of Medicine found that weekly injections of semaglutide (the active ingredient in Wegovy and Ozempic) reduced the risk of heart attack and stroke in patients with overweight or obesity if they had pre-existing cardiovascular disease even if they didn't have diabetes.
Managing High Blood Pressure
Managing High Cholesterol
Read the original article on Verywell Health.

