What Is Colitis?
There are many causes of inflammation in the colon
Medically reviewed by Jay N. Yepuri, MDMedically reviewed by Jay N. Yepuri, MD
Colitis is when the inner lining of the colon (large intestine) is inflamed due to infection or disease. The inflammation can cause swelling and ulcers as well as other symptoms, depending on the cause.
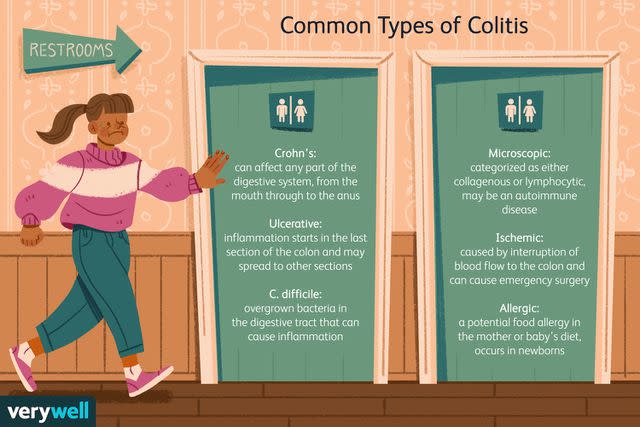
Some common conditions that cause colitis include inflammatory bowel disease (which includes Crohn’s disease and ulcerative colitis), Clostridioides difficile colitis, microscopic colitis, ischemic colitis, and allergic colitis.
Verywell / Theresa Chiechi
The colon is part of the digestive tract and the biggest part of the large intestine. The parts of the large intestine are the cecum, colon, rectum, and anus. It is a hollow tube between the small intestine and the rectum, where water and a few vitamins and minerals are absorbed from stool.
The colon is described as having four sections: the ascending colon, transverse colon, descending colon, and sigmoid colon.
Types of Colitis
These are common types of colitis.
Crohn’s Colitis
Crohn’s disease is one form of inflammatory bowel disease (IBD). This disorder can affect any part of the digestive system, from the mouth through to the anus. There are different forms of Crohn’s disease, based on where the inflammation is located.
When the disease is located in the large intestine, it is called Crohn’s colitis. Crohn’s that affects only the colon is found in about 20% of all people with the disease.
Ulcerative Colitis
Ulcerative colitis is a second form of IBD. This type affects only the large intestine. The colon and the rectum may be inflamed. Any segment of the colon can be involved, but the disease starts with inflammation in the last section and may spread up the colon to the other sections.
C. difficile Colitis
Clostridioides difficile (C. difficile, formerly known as Clostridium difficile) is a bacteria that normally lives in the digestive tract. However, some conditions can cause this bacteria to overgrow. C. difficile releases toxins, and in small amounts, it doesn’t cause illness. However, too much of the toxin in the colon can cause inflammation.
Microscopic Colitis
Microscopic colitis has two forms: collagenous colitis and lymphocytic colitis. It is not well understood, but there are theories that it may be an autoimmune condition, related to infection with a bacteria or virus, or caused by the use of certain medications.
The colon may look normal during a colonoscopy, but inflammation might be seen in collagenous colitis.
Ischemic Colitis
Ischemic colitis is caused by an interruption to the blood flow to the colon. It can happen quickly or slowly over time. This condition can be an emergency because, without blood flow, the tissue of the colon may start to die, in which case it would need to be removed through surgery.
Allergic Colitis
A condition that’s present in newborns, this form of colitis is thought to be caused by a food allergy. Some of the more common allergies that have been identified are cow’s milk, soy, egg, rice, and wheat. These may be in the diet of the breastfeeding parent or the baby.
Colitis Symptoms
The signs and symptoms of colitis will depend partly on the reason for the colitis and whether it is from an infection, a chronic illness, or is self-limiting (will eventually resolve).
Some of the more general signs and symptoms of colitis can include:
Abdominal cramps
Abdominal pain
Blood in the stool
Diarrhea (with or without blood)
Other symptoms are going to be more specific to the type of colitis. For instance, Crohn’s disease and ulcerative colitis may also be associated with symptoms outside the digestive system. Some of these other signs and symptoms might include:
Abdominal bloating
Aphthous ulcers (ulcers inside the mouth)
Chills
Dehydration (which may be associated with diarrhea)
Eye inflammation
Fatigue
Fever
Joint pain
Skin problems
Weight loss
Vomiting
Causes
The cause of the colitis is different for each type:
Crohn’s disease and ulcerative colitis: The cause is unknown, but there is known to be a genetic (inherited) component and thought to be one or more environmental triggers.
C. difficile colitis: This type of colitis is caused by an overgrowth of the C. difficile bacteria, which could occur after treatment with certain types of antibiotics.
Microscopic colitis: The causes of microscopic colitis are not understood, but women over 50 are affected more often.
Ischemic colitis: This condition is caused by a lack of blood flow. The cause could be a blood clot, plaque buildup in an artery, scar tissue in an artery, or narrowed blood vessels caused by a drug.
Allergic colitis: This condition is found in infants and is most often associated with a food allergy. In some cases, the bleeding will resolve when the food is removed from the diet. In other cases, it may stop spontaneously.
Diagnosis
Inflammation in the colon might be seen with an endoscopy, where the lining of the colon can be seen by various methods. This can be a colonoscopy, where a flexible tube with a camera and a light on the end is inserted up through the anus and into the colon.
A flexible sigmoidoscopy is another method. It can’t be used to see higher up in the colon but only the first section. A third method is capsule endoscopy, which is completed by swallowing a small camera that sends images of the colon.
A stool sample might be needed to either confirm or rule out an infection, such as with C. difficile. Blood work might also be helpful. It may not help in diagnosing the cause of the colitis, but it can help the doctor to understand if there are increased levels of white blood cells or if the red blood cell count is low from blood loss.
In some cases, other tests might be used that can show if the walls of the colon have become thickened because they are scarred or inflamed. This includes:
Treatment
How the colitis is treated will depend on the cause. In some cases, it can be treated and then resolved. But in others, the condition might be considered chronic, and will be long-lasting.
IBD
IBD is an immune-mediated condition that is lifelong. Crohn's disease and ulcerative colitis might be treated with 5-aminosalicylic acid medications (5-ASA), corticosteroids, immunomodulators, and biologics. Lifestyle changes, such as diet and stress reduction, might be used as well.
Complementary and alternative therapies, vitamins, minerals, and supplements might be used to treat the various signs and symptoms of the disease or its effects.
Microscopic Colitis
Cholestyramine, 5-ASA drugs, corticosteroids, immunomodulators, and anti-tumor necrosis factor alpha drugs have all been studied for use in treating microscopic colitis, with varying results. There are also case reports of surgery (colectomy with ileostomy placement) used to treat this condition, but it is not common.
Ischemic Colitis
If the cause is from a medication, such as one that constricts the blood vessels, stopping the drug might be part of treatment. Antibiotics, pain relief medications, and intravenous fluids might also be given in the hospital.
For serious or life-threatening cases of this condition, surgery to repair the damage to the arteries or to the parts of the colon that are affected might be needed.
C. difficile Colitis
The treatment of C. difficile infection can get tricky because it is usually treated with antibiotics, including Vancocin (vancomycin), Xifaxan (rifaximin), and Dificid (fidaxomicin). Resistance to antibiotics, however, is an increasingly difficult problem and can affect treatment decisions.
Fecal microbiota transplantation (FMT), where stool from a healthy donor is placed in the colon of someone affected by a C. difficile infection, is also used. In 2022, the FDA approved Rebyota, the first fecal microbiota product, and in 2023, Vowst, the first fecal microbiota product taken orally. Rebyota and Vowst are approved for the prevention of the recurrence of C. diff infections in adults who have completed antibiotic treatment for recurrent C. diff infections.
Probiotics have not shown many results in treating the infection but might also be used, along with other therapies.
Allergic Colitis
If there’s thought to be a food allergy at the source of the inflammation or bleeding, removing one or more foods from the diet of the baby and/or the breastfeeding parent might be the treatment.
In some cases, a special elemental formula, which doesn’t contain any of the most common proteins that cause allergy, might be given to the baby instead of breast milk or the formula given previously.
Prognosis
The prognosis varies by the type of colitis.
IBD
Crohn’s disease and ulcerative colitis are chronic, lifelong conditions. However, most people have mild or moderate disease that can be controlled with available medical therapies. Some patients experience severe disease and need hospitalizations, surgery, or experience complications.
Patients should keep in close contact with their physicians to keep up with treatment and understand their individual risk of complications.
Microscopic Colitis
Microscopic colitis can be chronic, but many patients achieve remission with treatment. Usually, medication needs to be continued because when it is stopped, symptoms may crop up again. There are rare cases where the condition doesn’t respond well to treatment, and surgery or biologics are needed.
Ischemic Colitis
Overall, the prognosis for ischemic colitis is good. However, it will be highly dependent on the cause, how extensive the damage is, and which part of the colon is affected. This condition can be fatal, but that is rare and usually when the entire colon is affected and surgery is needed. However, the majority of people recover without needing surgery.
C. difficile Colitis
Unfortunately, C. difficile infections are becoming increasingly difficult to treat because of antibiotic resistance. Some patients have recurrent infections because it can be difficult to eradicate all the bacteria.
There is ongoing study to find combinations of antibiotics that may help patients clear the infection and newer treatments like fecal microbiota transplantation.
Allergic Colitis
In most cases, allergic colitis is self-limiting and will resolve on its own. Blood in the stool is upsetting for caregivers, but fortunately, it rarely leads to anemia. There may be treatments given, such as changes to diet, with supplements being given when needed.
Most babies do well, and the colitis and bleeding resolve by the time they’re a year old. At that time, any food that was restricted is reintroduced into the diet.
Coping
The symptoms of colitis can be distressing. Blood in the stool is never normal and is always a reason to seek medical attention. There are many different possible reasons for abdominal pain and bleeding, which can be confusing and make the diagnosis process long.
In some cases, the reason for colitis can be treated and it doesn’t occur again. In others, however, it can be chronic and lifelong. It can be distressing to learn that a condition can’t currently be cured but needs ongoing medical treatment. Living with unpredictability can be difficult.
For some causes of colitis, treatment might include changes to diet. A referral to a registered dietitian can help in learning how to manage diet in the long and short term. This can also ensure that there are enough vitamins and nutrients in the diet.
Support groups can also be a significant source of information. Connecting with others who live with the condition or who are caregivers is a way to learn how to live a better quality of life and understand more about treatments.
Patient advocacy groups are good resources, as well as those that are put together by hospital systems or physicians.
Summary
Colitis is inflammation of the lining of the colon. Common types include inflammatory bowel disease, Clostridium difficile colitis, microscopic colitis, ischemic colitis, and allergic colitis. These often have symptoms such as diarrhea, abdominal pain, cramps, and blood in the stool.
The diagnostic process will often include imaging. Treatment will depend on the type but could include medication, surgery, and lifestyle changes.
A Word From Verywell
No matter the reason for the colitis, it can be a disruption to your life to get a diagnosis and treatment. It may be difficult to talk about bloody stools, diarrhea, and other digestive system problems. Still, it’s important to tell healthcare professionals about all the signs and symptoms.
There will be various emotions that come along with being diagnosed with a digestive condition, whether it is chronic or acute in nature. It may be helpful to connect with a therapist or social worker to work through processing everything.
Read the original article on Verywell Health.

