What You Need to Know About Psoriatic Arthritis and Pernicious Anemia
Symptoms, risk factors, multiple autoimmune conditions, treatment, and more
Medically reviewed by Susan Bard, MD
Pernicious anemia (PA) is often thought of as a disease that older people get, but, actually, it can affect people of all ages. Research shows it is strongly associated with other autoimmune diseases, including psoriatic arthritis (PsA), a type of inflammatory arthritis that can affect people with psoriasis (an autoimmune skin condition).
According to the Pernicious Anaemia Society, PA affects up to 4% of people with psoriatic arthritis. Symptoms of PsA include joint pain, stiffness, and swelling that flares up and subsides. PsA also causes low red blood cell counts, which is a sign of anemia.
Keep reading to learn more about these two conditions, risk factors, treatment, and more.
What Is Pernicious Anemia?
The term anemia refers to medical conditions in which the body can't make enough healthy red blood cells to transport oxygen.
Pernicious anemia is a type of anemia mainly caused by an autoimmune process that attacks the cells that produce intrinsic factor, a substance the digestive system needs to absorb vitamin B12 from food.
Intrinsic factor is needed to absorb dietary vitamin B12 in the small intestine. Vitamin B12 is an essential vitamin, and you need it to allow for proper red blood cell production and function, as well as to keep nerve cells healthy.
How Common Is Pernicious Anemia?
PA is extremely rare, affecting about 0.1% of the general population and 1.9% of the population older than age 60. PA is also the reason for up to 50% of cases of vitamin B12 deficiency in adults.
The term “pernicious” means deadly, and this type of anemia is called pernicious because it was considered fatal in the past. These days, the condition is easily treatable with vitamin B12 supplementation—either in pill form or B12 injections. If PA is left untreated, though, it can lead to very severe complications, including neurological problems.
Symptoms
Pernicious anemia progresses slowly, which makes it harder to recognize. Most people get used to the symptoms and don’t realize there is a problem.
The most common symptoms of PA are:
Additional symptoms include appetite loss, heartburn, constipation, nausea, and vomiting.
Risk Factors for Pernicious Anemia
Some people have a higher risk for pernicious anemia. This includes those with a family history of the condition and people of Northern European or Scandinavian backgrounds.
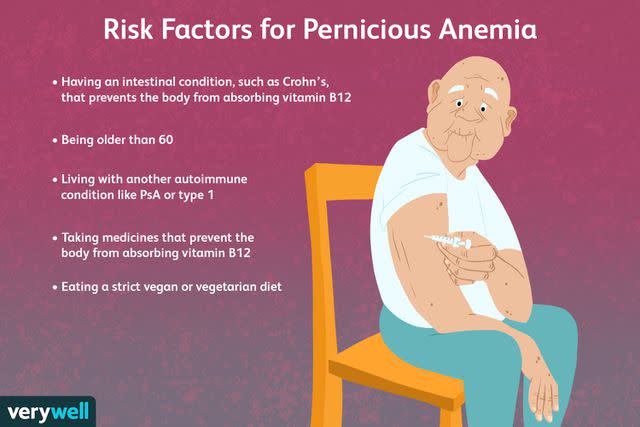
Verywell / Laura Porter
Additional risk factors associated with PA include:
Being female, as in one study, 81% of participants with PA were female
Having another autoimmune condition like PsA or type 1 diabetes
Having had part of your stomach removed
Being older than age 60
Having an intestinal condition that prevents the body from absorbing vitamin B12, such as Crohn’s disease (inflammation of the digestive tract)
Taking medicines that prevent the body from absorbing vitamin B12, including antibiotics and medications to treat diabetes or seizures
Being a strict vegetarian or vegan who doesn’t eat animal products, including dairy, and who doesn’t take B12 supplements, as well as someone who doesn’t eat a healthy and balanced diet
Having a tapeworm infection, as tapeworms feed off of vitamin B12 in the small intestine; tapeworm infections are caused by ingesting food or water contaminated with tapeworm eggs or larvae.
The autoimmune process that causes PA cannot be prevented. Vitamin B12 deficiency linked to other conditions (such as gastrointestinal diseases) is preventable to the extent those conditions also can be prevented. If vitamin B12 deficiency is related to diet, PA can be prevented with oral B12 supplements.
Multiple Autoimmune Conditions
It is not uncommon for people to have more than one type of autoimmune disease. In fact, people with PsA, psoriasis, rheumatoid arthritis (RA, which attacks the joints), and many other autoimmune diseases carry a higher risk of developing another autoimmune disease.
Although some conditions are more likely to coincide with another, the likelihood that someone with an autoimmune disease will develop another autoimmune disease is high.
Researchers believe autoimmune diseases co-occur for a variety of reasons. One theory is that when the immune system already has an autoimmunity issue, it is vulnerable and, therefore, open for another autoimmune disease to develop.
Genetic factors might contribute to the development of multiple autoimmune diseases, as well. Researchers believe that certain genetic and environmental factors can disrupt the immune system in a way that sets the stage for additional autoimmune disorders to progress.
A 2021 report in the journal Nature Communications reported that up to 55.8% of people with pernicious anemia have at least one other autoimmune disorder. Up to 40% of people with PA also have rheumatoid arthritis—a condition caused by similar inflammatory processes to PsA.
According to the same report, other autoimmune conditions that occurred concurrently with PA included type 1 diabetes (in which the pancreas doesn't make enough insulin, 35.9%), vitiligo (when the skin loses its pigment, 37.9%), and Hashimoto’s thyroiditis (which damages the thyroid, 33.7%).
The risk for pernicious anemia in people with psoriatic arthritis isn’t clearly reported in literature. However, the risk for pernicious anemia associated with psoriasis appears to be high, at around 28%, according to the Pernicious Anaemia Society.
The research shows that psoriasis belongs to a group of disorders that tend to appear together and include both pernicious anemia and psoriasis. And according to the National Psoriasis Foundation, up to 33% of people who have psoriasis also have PsA, which further adds to their risk of pernicious anemia.
Multiple Autoimmune Syndrome
When three or more autoimmune diseases occur in the same person, it is called multiple autoimmune syndrome. Oftentimes, at least one of these diseases is an autoimmune skin condition.
Treatment
The symptoms of PA and vitamin B12 deficiency can be managed by replacing vitamin B12 in the body. But the vitamins you find at the drugstore won’t be enough. Your doctor will need to prescribe vitamin B12 injections to manage your vitamin B12 deficiency.
Your doctor or a nurse can give you a vitamin B12 shot in a muscle. The injections are either given daily or weekly, depending on the severity of your PA.
Vitamin B12 oral supplements are rarely prescribed for PA as they don't work as well as injections. A 2016 review in the journal Frontiers in Medicine found them to be less effective than B12 shots. The study’s authors noted that many people might prefer taking oral supplements, however.
You may start to see improvements within a few days or weeks after you start treating your PA. Even after your B12 levels improve, your doctor may recommend you keep getting vitamin B12 injections on a monthly basis. At this point, you can self-administer shots at home or with the help of a family member to reduce your trips to the doctor.
In addition to treating the pernicious anemia, if your doctors can find an underlying cause, they will work to get that condition under control. This is generally the case when the body’s small intestine cannot properly absorb vitamin B12, as can happen with conditions like celiac disease (an intolerance to the gluten found in wheat and other grains), Crohn’s disease, and other types of inflammatory bowel disease (IBD).
If your B12 levels remain stable, your doctor might suggest supplements instead. However, depending on how deficient you are in intrinsic factor, you may be required to get B12 injections as a sole treatment for PA.
Pernicious anemia needs to be treated because it can lead to life-threatening complications without treatment. Talk to your doctor about your treatment options and how having PsA can contribute to complications of PA.
Summary
Pernicious anemia, which is caused by a vitamin B12 deficiency, may occur more often in people with other autoimmune diseases, including psoriatic arthritis. The condition needs to be treated with vitamin B12 to prevent serious complications.
A Word From Verywell
Most people with pernicious anemia will need lifelong treatment with B12 injections or supplements. They will also need lifelong monitoring. These are the best ways to prevent long-term complications from PA.
Talk to your doctor if you think you are experiencing symptoms of pernicious anemia or symptoms that may be related to psoriatic arthritis. Early diagnosis, treatment, and monitoring are all vital for preventing future problems and complications of PA.
Frequently Asked Questions
How do you treat pernicious anemia?
Doctors treat pernicious anemia by replacing vitamin B12 in the body. Once a person has been diagnosed with the condition, they will need lifelong treatment. Treatment of PA aims to prevent or treat anemia and its signs and symptoms, prevent complications, and treat underlying causes if a cause can be determined.
How is pernicious anemia diagnosed?
A diagnosis of pernicious anemia is based on your medical and family histories, a physical exam, and blood work. Doctors will also determine if your PA is related to a lack of intrinsic factor or if there is another cause. They will want to find out how severe that underlying condition is in order to treat it and get it under control.
If the diagnosis is uncertain, your doctor might suggest a bone marrow test. Bone marrow testing can tell your doctor if your bone marrow is healthy and making enough red blood cells. With PA, the bone marrow cells that turn into blood cells are larger than normal.
What causes psoriatic arthritis flare-ups?
Just about everyone with psoriatic arthritis has flare-ups—periods where symptoms of the condition are worse than usual. Common PsA and psoriasis triggers include:
Skin trauma or injury, including dry skin, sunburns, cuts, bumps, bruises, scratches, or scrapes
Stress
Alcohol consumption
Weather changes, including cold, dry weather, and lack of sunlight
Certain medications, including antimalarial drugs, beta-blockers, and lithium
Excess weight that puts stress on joints
Smoking
Gluten
Common infections, including upper respiratory infections and strep throat
Related: An Overview of Psoriatic Arthritis Triggers
Read the original article on Verywell Health.

