The real reason you get menopause brain fog – and what you can do about it

I am turning 40 and honestly – really – I feel fine about my ageing body. My husband and I will grow more wrinkled and stooped in tandem. That seems fair enough. A growing field of research, however, suggests that as we enter into this new midlife phase, my brain will begin to age, change and decline in ways that his will not. And this inequality is the straw that broke the camel’s back or, if you will, the symptom that snapped my peri-menopausal patience.
If my husband and I sat down to take a verbal memory test today, it’s quite likely I would trounce him. If we sat the same test in around a decade’s time, however, the tables might turn. On average, adult women perform better than men at such skills, explains Jill Goldstein, a professor of psychiatry and medicine at Harvard Medical School, and the founder of the Innovation Center on Sex Differences in Medicine at Massachusetts General Hospital.
That advantage, however, narrows during the menopause. Prof Goldstein’s own work has probed some of the reasons for this. “We’ve shown that, for women in early midlife, the importance of reproductive age is distinct from chronological age, whereas for men in early midlife, it is chronological age that drives memory changes,” she explains.
Brain changes during the menopause
The influence of sex hormones – oestrogen, progesterone and testosterone – are not confined to our reproductive organs, explains Prof Goldstein. There are receptors for these hormones in “critical brain regions that regulate mood, anxiety, stress response, memory, and appetites,” she says. In fact, these hormones can affect the way your brain cells develop, connect with one another, and even die.
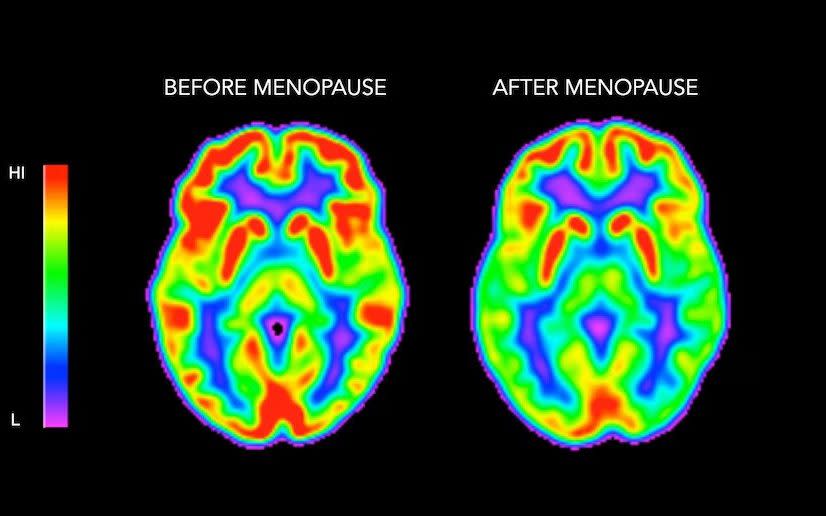
Prof Goldstein’s research shows that, in menopause, declines in estradiol – the most potent and abundant form of oestrogen during a woman’s reproductive years – result in “a reorganisation in the brain circuitry that regulates memory performance, impacting how we process information, remember things, and even how we feel physically and emotionally”.
Find yourself forgetting the keys, or calling the kids by the dog’s name? Blame estradiol.
Brain fog is more common than hot flushes
For centuries, women have been given a narrow script of what menopause entails; one that suggests that it lasts just 12 months from our last period and will leave us engulfed in hot flushes and night sweats.
Dr Louise Newson is a menopause specialist and author of The Definitive Guide to the Perimenopause & Menopause. This, she suggests, is a wholly inadequate picture.
When Dr Newson surveyed nearly 6,000 women, most common symptoms reported were not the classic hot flushes or sweats, but symptoms stemming from the brain and nervous system.
“Brain fog, low energy, memory problems, sleep problems, low mood, low libido, irritability, low motivation, crying or tearfulness, feeling nervous, low concentration, mood swings, headaches...”
All in all, “I think menopause should be reframed as a neurological condition really, not a gynaecological one,” says Newson.
Brain changes begin long before the menopause
Not only that, the time frame is much longer than we are generally led to believe. Plummeting hormones may start to affect women’s brains from their early 40s on.
A Finnish study subjected 43 men and 28 women to MRI brain scans, first at an age of between 33–35, and then again between the ages of 42–44. They found the women had lost more brain volume over that interval than the men. The researchers suggested that this could be down to the neuroprotective effects of testosterone. But also the fact that hormonal changes that lead to the menopause begin many years prior to the final menstrual period.
“Often testosterone levels decline first,” Dr Newson explains. “We see a lot of women [in the clinic] with symptoms like lowered mood, memory problems and poor sleep. On measuring them, we find their testosterone levels are really low.” Once they are prescribed testosterone their clarity and focus improve.
“Menopause changes the brain’s structure, functionality, and even its connectivity in fairly unique ways,” confirms Dr Lisa Mosconi, a neuroscientist, the director of the Weill Cornell Women’s Brain Initiative and the author of The Menopause Brain.
In 2021, she found that women can experience a decline in grey matter, the part of brain cells that process information, during peri and early menopause. White matter (the fibres that connect those cells) also declines, as does the brain’s consumption of glucose, the principal fuel source for cells.
Like the Finnish study, Dr Mosconi’s research suggests that women’s brains begin reacting to hormonal variation years before those that we typically associate with the menopause, and in some really quite profound ways.
Alzheimer’s affects twice as many women as men. This is partly explained by their longer average life span. Still, Dr Mosconi’s study found that women with a particular genetic risk factor for Alzheimer’s disease (a variant of the APOE gene) begin to develop amyloid plaques that are linked to the disease from their late 40s onwards.
“Oestrogen has neuroprotective qualities, and its reduction during menopause could make the brain more vulnerable to Alzheimer’s disease,” she explains.
The positive brain changes post-menopause
All of this makes my next decade sound pretty bleak. Thankfully, there is far better news. Some of the declines identified in Dr Mosconi’s study proved to be temporary, reversing post-menopause. Plus, she says: “Menopause is actually a renovation project on the brain. All those neurons and connections between neurons that were needed to support ovulation and enable a pregnancy are no longer needed and can be discarded. It’s the brain’s chance to get ‘leaner and meaner’, if you will. This can lead to some glitches, but also has some advantages.”
Some research suggests that post-menopausal reductions in hormonal fluctuations can lead to renewed emotional wellbeing and sense of fulfilment for some women, says Dr Mosconi. The amygdala, the brain’s emotional centre, can become less reactive to negative or upsetting experiences, while some women report feeling more liberated or a new sense of clarity and focus.
There are, the experts assure me, many ways to come through the menopause with a mighty powerful brain. “Postmenopausal women are no longer reproductive, but they can remain markedly productive,” Dr Mosconi notes. “Effortful cognitive exercise, effortful physical exercise, and social contact,” lists Prof Goldstein. “These are the three primary things that can help to keep your brain intact as we age.” So exercise your body and brain, and make time for your friends. That is a prescription I can get behind.
How to improve your menopausal brain
By Dr Lisa Mosconi
Diet: Emphasise a Mediterranean-style diet rich in omega-3 fatty acids, fruits, vegetables, whole grains, and lean protein. High blood sugar, diabetes, belly fat, and a heart age score greater than your actual age during midlife were associated with a significant decline in the time it took women to do a mental task a decade later, according to a 2021 analysis.
Hormone replacement therapy (HRT): Dr Mosconi’s research suggests HRT is associated with larger grey matter volume in women during midlife. Grey matter runs throughout the nervous system and is key to memory, decision-making and emotions.
Exercise: Regular physical activity, including aerobic and resistance training, can improve hormonal function, cognitive function and overall brain health. Aerobic exercise has been shown to increase levels of the protein BDNF higher levels of which are associated with less brain change in menopause.
Cognitive engagement: Engage in activities that challenge your brain, such as learning a new language, playing musical instruments, or solving puzzles.
Sleep: Aim for seven to nine hours of quality sleep per night, as sleep is crucial for cognitive health and memory consolidation.
Stress management: Techniques such as mindfulness, meditation, or yoga can reduce stress and its negative effects on the brain.
Regular medical check-ups: Work with your doctor to manage any medical conditions that can impact brain health, from heart disease to diabetes and thyroid disease.
Pharmacological options: Discuss hormonal and non-hormonal options with a healthcare professional.

