Tooth Abscess: Everything You Need to Know
Types, causes, symptoms, and treatment
Medically reviewed by Brian T. Luong, DMDMedically reviewed by Brian T. Luong, DMD
A tooth abscess, also called an oral or dental abscess, is a localized bacterial infection in which pus builds up in a tooth, gum, or jawbone. The infection can affect surrounding tissues and cause severe pain.
A tooth abscess needs appropriate treatment, which can improve symptoms within days. Left untreated, it can lead to hospitalization or become life-threatening. Treatment options for a tooth abscess include surgical drainage, root canal, tooth extraction, and antibiotics.
This article will cover the symptoms and causes of tooth abscesses, how they are diagnosed, available treatment options, and more.
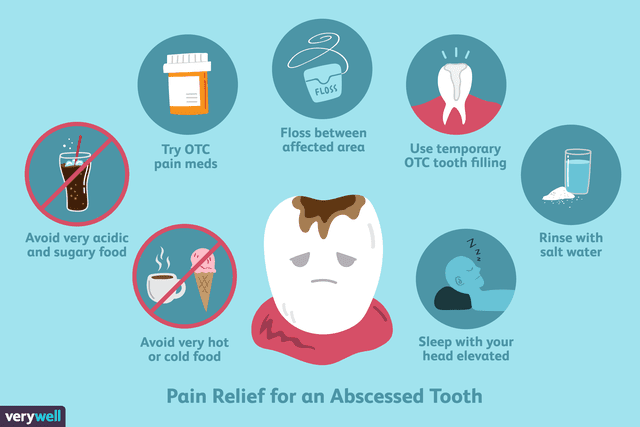
Illustration by Joshua Seong. © Verywell, 2018.
Types of Dental Abscesses
Dental abscesses can affect the teeth and gums. The three most common tooth abscess types are periapical abscess, periodontal abscess, and gingival abscess.
Periapical Abscess
A periapical abscess forms at the tip of the root of a tooth. It results from a dental injury or cavity. It is one of the most common dental emergencies.
This abscess type affects the top part of the tooth. It results from a bacterial infection of the pulp—the innermost layer of a tooth containing the nerves, blood vessels, cells, and connective tissues that provide the tooth with nutrients.
An infection of the tooth pulp can spread to a nearby tooth or root and cause systemic symptoms such as fever or malaise (a general feeling of unwellness).
Periodontal Abscess
A periodontal abscess affects the bones and tissues that support the teeth. It generally results from periodontitis, a severe type of gum disease that can lead to tooth loss.
A periodontal abscess will usually present with swollen red gums (related to periodontal disease), The surrounding teeth may not be broken down with large cavities. This is in contrast to periapical abscesses, which can be associated with large cavities and broken-down teeth.
Periodontal abscesses share a microbiology like that of periodontal disease— inflammation and infection of the gums and the bone that supports your teeth. Most of the bacteria involved are resistant to antibiotics (except for azithromycin).
Periodontal Disease vs. Periodontitis
Periodontal disease refers to any condition that affects the teeth, gums, bone foundations, and ligaments. Gingivitis is the earliest stage of periodontal disease, while periodontitis is a more severe condition that damages soft tissue and bone.
Gingival Abscess
Gingival abscess, also called gum abscess, develops in the gums but generally does not affect the teeth.
This type of abscess can be painful and lead to severe complications, including an infection that can spread deeper into the gum tissue and travel to other parts of the face and body.
Tooth Abscess Symptoms
The main symptom of a tooth abscess is throbbing near the affected tooth in the gums. The pain will come on suddenly and get worse over time.
The pain will be continuous and may radiate into the jaw, ear, and neck. You may feel pain when biting and chewing and have facial swelling and redness or discoloration. Tooth abscess pain can be described as throbbing, shooting, gnawing, or sharp.
Related: Tooth Pain: Causes, Treatment, and When to See a Dentist
Additional symptoms of tooth abscess may include:
A bitter taste in the mouth
Bad breath
Sensitivity to hot or cold
Swelling of the gums over the affected tooth
Swollen neck glands
Fever
Malaise
Stages of Developing a Tooth Abscess
Five stages of tooth decay can lead to the development of a tooth abscess: white spots, enamel decay, dentin decay, pulp involvement, and abscess formation.
White spots: These are a sign of enamel demineralization or the start of a cavity.
Enamel decay: Untreated white spots will lead to enamel decay, by which the cavity has started to work its way into the tooth.
Dentin decay: At this stage, decay has progressed to the layer beneath the tooth enamel. You may notice pain and sensitivity at this stage or see a visible hole or cavity in the tooth.
Pulp involvement: This stage is when bacteria get into the deep layers of the tooth. Bacteria may also attack the tooth nerve, causing intense pain.
Abscess formation: An abscess occurs in the later part of the tooth decay when bacteria make their way to the tooth pulp and go deep into the gums and jawbone. At this point, you will start to experience symptoms of an infection, including fever.
What Causes an Abscessed Tooth?
If you are not brushing regularly, bacteria will build up in and around your gums and teeth, leading to an abscess.
Other risk factors for tooth abscess include:
An injury or dental damage: A broken tooth from an injury or a deep tooth crack can allow bacteria to get into deeper parts of your gums and teeth.
Eating sugary and highly processed foods: These foods often lead to dental plaque buildup. If you do not properly brush and floss, gum disease and tooth decay will develop. These can eventually advance to a dental abscess.
Dental procedure: Sometimes, a dental procedure can lead to a periodontal pocket, a tiny gap that forms when a periodontal ligament separates from the root. That pocket is hard to keep clean, and bacteria will build up, eventually progressing into a periodontal abscess. A periodontal abscess can also occur following a perforation of a tooth by an endodontics (dental) instrument or an impaction of a foreign object, such as a toothbrush bristle.
Who’s More Likely to Develop an Abscessed Tooth?
Some people are at a higher risk for an abscessed tooth. This includes people who:
Smoke: Your risk for a dental abscess is higher if you are a smoker. Research shows that smoking has a negative effect on dental health and can lead to dental problems and infections.
Have weakened immune systems: People with weakened immune systems are at a higher risk of developing dental abscesses. This includes people who are undergoing chemotherapy, take corticosteroids, or have diabetes.
Have a dry mouth: Xerostomia (a dry mouth) can also affect the healthy balance of bacteria in the mouth, eventually leading to decay, infections, and abscesses.
Have poor dental hygiene: If you do not regularly brush and floss and get dental cleanings, bacteria can build up in your teeth and gums, leading to dental problems.
Related: Toothache: Symptoms, Causes, and Treatment
How Is an Abscessed Tooth Diagnosed?
If you experience symptoms of a gum or tooth abscess, make an appointment with a dentist as soon as possible.
A dentist can examine your gums for signs of infection, including swelling, tenderness, and redness. The dentist may also order a dental X-ray to look for a pulp infection, periodontal disease, or bone loss related to the infection.
Your dentist might request a pulp vitality test to check the strength and overall health of pulp tissue and determine your treatment options. This is recommended for both people with dental pain and those without or those who report hot or cold sensitivity in specific areas of their mouth.
If the Tooth Abscess Bursts
If the tooth abscess bursts, you may feel immediate pain relief. But you may also notice a foul taste and smell in your mouth due to pus drainage. You should still contact a dentist to treat the infection.
How Is an Abscessed Tooth Treated?
The goals of treatment for a tooth abscess are to clear the infection, save the tooth, and prevent complications, such as the loss of the tooth.
Treatment options include:
Incision and drainage of the abscess: If the abscess is treated early and has not progressed, an incision and drainage procedure is recommended. With this procedure, the dentist cleans the affected area and then makes a minor incision to drain the pus. After the abscess is cleaned and drained, the dentist will prescribe antibiotics to properly treat the infection.
Root canal: A root canal might be necessary if the bacteria spread to the dental pulp and tooth root. A root canal might also treat a periapical abscess at the root of a tooth.
Extraction of an affected tooth: A tooth extraction might be necessary if the tooth cannot be saved.
Antibiotics to control infection: Antibiotics are typically given after dental treatment of a tooth abscess. Antibiotics must be taken for the entire treatment duration to ensure the infection fully clears.
Related: How Long After Starting Antibiotics Will My Tooth Pain Go Away?
Abscessed Tooth Self-Care
A tooth abscess requires dental treatment, but some home remedies can relieve pain and discomfort as the mouth heals.
Saltwater rinses: Rinsing your mouth with salt water can offer temporary pain relief and even promote healing. Mix a teaspoon of salt with a lukewarm glass of water and rinse your mouth with it. You will want to swish the solution around in your mouth for at least 30 seconds and then spit it out.
Cold compresses: A cold compress can help alleviate pain and swelling. Wrap ice cubes in a dry towel and hold the compress against the skin near the affected area. Repeat the process for 15-minute intervals multiple times a day.
Keep your mouth clean: Brush teeth at least twice daily and floss once daily. Consider using an antimicrobial mouthwash to help prevent the infection from spreading.
Avoid smoking and alcohol: It is a good idea to avoid cigarette smoking or drinking alcohol until you have seen a dentist. This can help you to avoid further decay and infection.
OTC Pain Relief for an Abscessed Tooth
If you are experiencing intense pain, you might be able to get relief with an over-the-counter (OTC) pain reliever like Advil or Motrin (ibuprofen) or aspirin. Make sure you only take the recommended dose and reach out to a dentist if you are still struggling with tooth and gum pain.
Root Canal and Endodontic Surgery
Root canals and tooth extractions are oral surgery procedures. Your general dentist typically would not do these procedures unless they have additional training and dental board certifications. You will likely be referred to an oral surgeon.
A root canal procedure involves removing the infected dental pulp. After the bacteria is removed, the root canal is filled, and the tooth is sealed. The tooth is then covered with a filling or dental crown.
If an abscessed tooth cannot be saved, it will need to be extracted (pulled). The procedure involves local anesthesia or sedation, and the tooth is removed using surgical instruments.
Can a Tooth Abscess Go Away On Its Own?
A tooth abscess will not go away on its own. The source of the infection needs to be removed and treated. An abscess must be drained and treated with antibiotics so the infection does not spread to other parts of the body, including the jaw, neck, and bloodstream.
If the tooth pulp is infected, a root canal and crown will be necessary. If a root canal cannot be performed, the tooth needs to be extracted.
Complications of an Untreated Tooth Abscess
If a tooth abscess is left untreated, the infection can spread. Some complications require hospitalization and can be life-threatening.
Complications of a tooth abscess include:
Osteomyelitis: This is an infection of the jawbone surrounding the affected tooth and can occur if a tooth abscess goes untreated.
Cellulitis: An untreated tooth abscess can lead to a skin infection of the soft tissue around the abscessed tooth.
Parapharyngeal or peritonsillar infection: An abscess that forms at the back of the mouth can lead to an infection of the throat, tonsils, or both.
Septic cavernous sinus thrombosis (CST): Though rare, a dental infection can lead to sinus infection, which in turn can lead to serious blood clots in the major veins that pass through the sinus and facial paralysis.
Sepsis: A dental infection could potentially travel to the bloodstream and lead to sepsis. Sepsis is a life-threatening infection that can lead to septic shock, blood clots, and organ failure.
Dentoalveolar abscess: If the infection travels to the orbit (the bony cavity of the eye), it can lead to an abscess of the orbit.
Brain abscess: An untreated tooth abscess infection can travel and spread to the brain. If an infection has spread to the brain, symptoms may include a stiff neck, fever, chills, and changes in vision and mental state.
Ludwig’s angina and mediastinitis: An untreated tooth abscess in the lower jaw could lead to a deep neck infection (Ludwig’s angina) or inflammation of the chest cavity (mediastinitis).
Do Not Put Your Health At Risk
Although the above complications are rare or uncommon, you should still contact a dentist if you have a tooth abscess. This way, you avoid putting your health at risk.
What’s the Outlook for Someone With an Abscessed Tooth?
When addressed promptly, the outlook for a person with tooth abscess can be positive. A dental procedure and antibiotics can cure a tooth abscess. You will typically feel pain relief and fully recover within weeks.
If you do not seek treatment for a tooth abscess, you could put yourself at risk of severe complications. If you suspect a dental abscess, reach out to a dentist right away. The sooner you get checked out and treated, the sooner your life can return to normal.
Can You Prevent a Tooth Abscess?
Preventing a tooth abscess requires good oral hygiene habits. These include:
Brush twice a day and after eating sugary or acidic foods and snacks.
Floss at least once a day.
Get regular dental cleanings (every six months) to clear up plaque and tartar and check for tooth decay and other dental problems.
Follow a healthy diet to prevent cavities and promote stronger teeth.
Change your toothbrush every few months and after you get sick.
Use fluoride toothpaste to help build strong enamel.
Don’t smoke. If you need help quitting, reach out to a healthcare provider. They can provide resources and information to help you quit for good.
Avoid trauma to your teeth, Wear mouthguards when playing sports, drive safely, and avoid situations that can result in trauma to your face.
When to Seek Emergency Care
If you have facial swelling, difficulty opening your mouth, or problems breathing, call 911 or go to your local emergency department. These symptoms might indicate the dental infection is spreading to your face or neck.
Confusion, an elevated heart rate, and problems swallowing are additional signs that may warrant an emergency room visit.
Summary
A tooth abscess is a localized bacterial infection in which pus builds up inside a tooth, the jaw, or the gums. The infection can spread to surrounding tissues and cause pain and swelling.
Tooth decay, gum disease, and trauma to the teeth or gums can cause tooth abscesses. Some people are at increased risk for dental abscesses, including smokers, those with poor dental hygiene, older adults, and anyone with a compromised immune system.
Without treatment, a dental abscess can spread to the jawbone, mouth, face, or neck. This can lead to severe and life-threatening complications.
If you experience signs of a tooth abscess or have dental pain, you should see a dentist right away. Treatment can manage the infection and its underlying cause.
Good oral hygiene is the best way to prevent tooth abscesses and other dental problems. You should see your dentist every six months for cleanings and dental screenings to address issues before they worsen.
Read the original article on Verywell Health.

