White Coat Syndrome and High Blood Pressure (HBP): What to Know
Many people experience stress and anxiety in healthcare settings, like hospitals or dental offices, which can lead to white coat syndrome. White coat syndrome is when blood pressure readings are high in a healthcare setting but normal at home. This condition is tricky to assess and can lead to a false high blood pressure (hypertension) diagnosis.
This article discusses how to identify white coat syndrome and manage it at home or in healthcare settings.
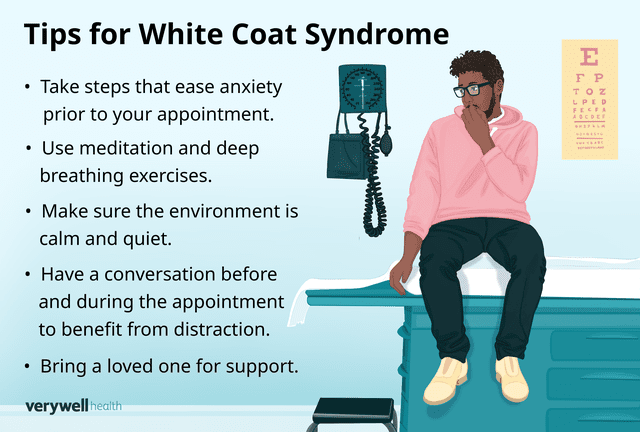
Illustration by Zoe Hansen for Verywell Health
Meaning of White Coat Syndrome
White coat syndrome occurs when blood pressure spikes in response to being seen by healthcare providers—who often wear white coats in clinical settings—or the clinical setting itself. Healthcare providers diagnose white coat syndrome by comparing blood pressure test results they take in the clinic to the results of readings taken at home.
In some people, white coat syndrome eases with repeat appointments as comfort and familiarity with the healthcare provider and setting grow.
When Is Blood Pressure High?
Blood pressure is the amount of force that blood exerts on the walls of your blood vessels. This measurement is divided into two numbers: systolic and diastolic blood pressure.
Systolic blood pressure is the pressure against blood vessel walls when the heart beats. It is the top number in a blood pressure reading.
Diastolic blood pressure is the pressure against blood vessel walls between beats when the heart is at rest. It is the bottom number in a blood pressure reading.
Experts have established ranges for low, normal, and high blood pressure:
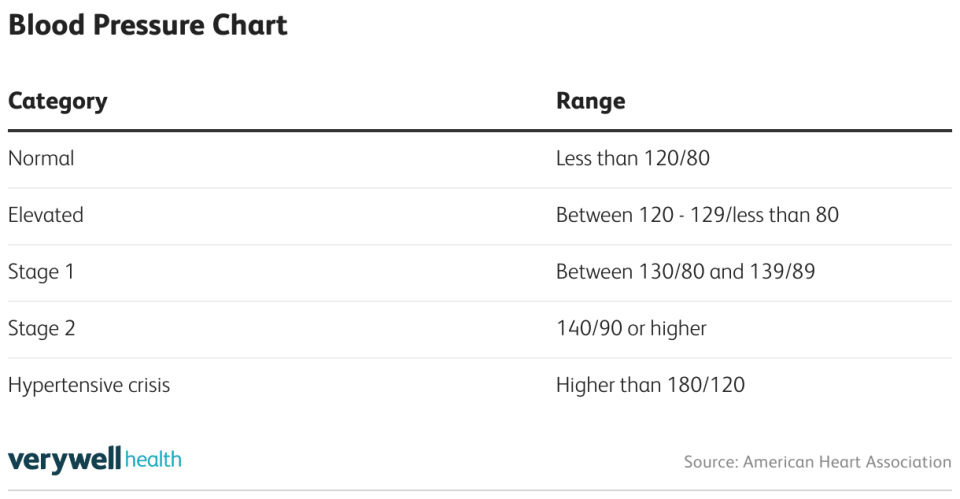
Having an elevated systolic blood pressure is a common sign of aging, so if you're 65 or older, a healthcare provider may consider a blood pressure of 130/80 normal. In contrast, children and adolescents tend to have lower blood pressure.
Frequency of HBP Readings
If you have a high blood pressure reading in a healthcare setting, your provider will recommend you return for a second test to confirm your condition. If the second test also shows high blood pressure, your provider may recommend home or “ambulatory” monitoring.
During ambulatory blood pressure monitoring, you wear a blood pressure cuff for 24 hours. Over the 24-hour period, the cuff automatically measures your blood pressure every 15 to 30 minutes and records the data. Your provider reviews the data to identify any concerning patterns.
While home blood pressure devices don’t replace in-clinic testing, they can help healthcare providers detect blood pressure differences that may occur due to white coat syndrome. Providers look for significant differences between repeated at-home and in-clinic test results to confirm white coat syndrome.
If healthcare providers suspect you have chronic high blood pressure, they may recommend in-office and ambulatory blood pressure monitoring every three to six months.
Associated Symptoms
High blood pressure and white coat syndrome usually do not cause symptoms. However, in severe cases, symptoms indicative of the two conditions include:
Changes in vision, visual disturbances
Difficulty talking or understanding speech
Gasping, shallow breaths, or other breathing difficulties
Numbness, physical weakness
Sudden headache
Sudden pain in the abdomen (belly area), chest, or back
If your home blood pressure monitor shows a hypertensive crisis (a reading of 180/120 or more) and you have no symptoms, check again in five minutes; if you get the same result, get emergency help. If you have a blood pressure reading of 180/120 accompanied by symptoms, call 911 immediately.
White Coat Syndrome: A Diagnostic Dilemma
White coat syndrome is a significant challenge for healthcare providers. It can lead to false diagnoses, and the condition may carry its own risks. Furthermore, some people have masked hypertension, a “reverse” white coat syndrome in which blood pressure lowers to healthy levels when in clinical settings, also presenting a challenge.
How Common Is White Coat Syndrome?
Though exact figures are unknown, studies suggest white coat syndrome is relatively common. Researchers found up to 30% of those with high blood pressure readings in clinical settings had normal results at home.
Unnecessary Prescriptions
The misleading readings due to white coat syndrome can lead to false or delayed diagnoses of high blood pressure. As a result, healthcare providers may start you on medications you don’t need or boost dosages when it isn’t necessary.
Unnecessary prescriptions can lead to side effects and negative health impacts. In addition, researchers found unnecessarily taking medications for high blood pressure lowered adherence to necessary medications.
Cardiovascular Risks
While white coat syndrome only causes temporary blood pressure spikes, it isn’t without cardiovascular risk. Researchers have found the following health risks associated with white coat syndrome:
Risk of hypertension: The overall risk of developing chronic hypertension is 2.5 times higher in those with white coat syndrome compared to those without.
Arterial stiffness: Researchers found associations between white coat syndrome and arterial stiffness (a reduced ability of heart arteries to expand and contract fully) in those with high blood pressure.
Cardiovascular risk: Though the exact relationship isn’t clear, the risk of heart problems in those with white coat syndrome is higher than in those without high blood pressure (but lower than in those with it), raising the rates of stroke, heart attack, and heart disease in this population.
Masked Hypertension
Masked hypertension is the inverse of white coat syndrome. It occurs when blood pressure readings in a clinical setting are within a healthy range when the patient actually has chronic high blood pressure. Masked hypertension can lead to delayed diagnosis or unnecessary changes in prescriptions. Untreated high blood pressure raises the risk of cardiovascular diseases, and masked hypertension is associated with organ damage.
Why Some People Experience White Coat Syndrome
Researchers believe white coat syndrome is a stress response to the hospital or clinical environment. It stimulates the sympathetic nervous system, triggering the fight-or-flight response, which releases adrenaline and other hormones and raises blood pressure.
Psychological factors also seem to play a role. In one study, researchers found that fear and anxiety about a healthcare provider detecting high blood pressure could even trigger white coat syndrome.
While everyone may be susceptible to white coat syndrome, certain populations are more likely to develop this condition. It occurs more often among women and people older than 50 (with increased prevalence with age).
How to Minimize White Coat Syndrome
The primary goal in alleviating white coat syndrome is to manage your body’s stress response. Blood pressure medications aren’t appropriate for this condition. Luckily, there are things you can do to address this condition at home and in your healthcare provider’s office.
At Home
Ambulatory blood pressure monitoring at home helps detect and manage white coat syndrome. Despite some limitations compared to in-office tests, checking your blood pressure at home or in a comfortable environment helps reduce the stress and anxiety that trigger white coat syndrome.
Learn and develop practices that ease anxiety and stress before taking your blood pressure at home. Such practices may include regular meditation or mindfulness exercises, deep breathing, or simply unwinding.
At a Provider Visit
There also are methods and strategies you can try in a healthcare setting to ease white coat syndrome, including:
Environment: Ask the healthcare provider to move you to a quieter area or room if it’s loud and busy. Try wearing headphones and listening to relaxing music.
Deep breathing: While seated or lying down, slowly inhale until your lungs are full. Hold the air in your lungs for a little while, then slowly exhale. Repeat several times.
Meditation: Close your eyes and focus your attention on an object, a set of words, or the act of breathing. Breathe slowly and calmly.
Conversation: Some people benefit from distractions; conversations before and during measurement may help take your mind off the stress and anxiety you typically feel in a healthcare setting.
Bring support: Bring a loved one or trusted friend to the appointment with you; ask your healthcare provider to have them accompany you during the test.
Managing Chronic High Blood Pressure
If you do have chronic high blood pressure—not white coat syndrome—it's important to manage and treat your hypertension to reduce your risk of cardiovascular conditions.
If you have elevated (between 120–129/less than 80) or stage 1 (between 130/80 and 139/89) hypertension, healthcare providers typically recommend lifestyle changes as the first-line approach. Lifestyle changes focus on improving cardiovascular health and taking on conditions that raise risk. Examples include:
Aiming for at least 150 minutes a week of light to moderate activity each week
Cutting down or quitting drinking alcohol
Emphasizing fruit, vegetables, healthy proteins, and vitamins—Dietary Approaches to Stop Hypertension (DASH) diet
Getting enough sleep, such as getting seven to eight hours a night and going to bed and rising at consistent times
Limiting salt intake
Maintaining a healthy weight by boosting exercise and dietary changes
Managing stress with meditation, exercises, yoga, or other activities
If lifestyle changes don't help lower your blood pressure, a healthcare provider will consider prescribing you medications. These should be taken daily, typically at consistent times. Your prescribing healthcare provider will offer more detailed instructions and monitor your blood pressure.
Medications for Hypertension
Healthcare providers prescribe several classes of medication for hypertension, which treat high blood pressure by opening up blood vessels or lowering the fluid content of blood. These medications include:
Angiotensin-converting enzyme (ACE) inhibitors, including Lotensin (benazepril) and Vasotec (enalapril)
Angiotensin 2 receptor (ARB) blockers, such as Edarbi (azilsartan) or Atacand (candesartan)
Calcium channel blockers, including Norvasc (amlodipine) and Calan (verapamil)
Diuretics like Bumex (bumetanide) or Aldactone (spironolactone)
Summary
White coat syndrome arises when you get abnormally high blood pressure readings in a healthcare setting. It is a stress reaction that causes blood pressure spikes that can make it seem as though you have high blood pressure when, in reality, they're temporary spikes.
Developing relaxation methods in the office or clinic and opting for home blood pressure monitoring can help you manage white coat syndrome. If you have high blood pressure, treatments include lifestyle changes and medications.
Read the original article on Verywell Health.

