ER workers ask state legislators to take steps to fix broken system
- Oops!Something went wrong.Please try again later.
BOSTON — It’s a chronic condition in Massachusetts hospitals: the lack of inpatient beds for people seeking care in emergency departments for acute conditions who end up boarding or staying in the departments for hours, days and even weeks, waiting to transfer to appropriate facilities.

“They have been seen in the emergency room, they need treatment, they can’t go home, and there’s no place else for them to go,” said Dr. Joseph Kopp, an emergency physician at Faulkner and Brigham & Women’s hospitals.
The lack of available beds affects the entire health care system and exacerbates other issues such as sicker patients who defer treatment due to the lack of a primary care physician, escalating workplace violence, and the lack of treatment options for people undergoing a behavioral health crisis or those with substance use disorders.
The unfolding Steward Health Care crisis could aggravate the lack of beds. Owner of eight Massachusetts hospitals, the company has filed for bankruptcy in Texas and plans to auction off its services. The hospitals are already losing staff and many lack adequate equipment and supplies.
While the emergency department physicians attending a legislative briefing Thursday acknowledged that three bills before the Legislature will not solve the problem, enacting them would be a big step forward to mitigate them.
Which bills are ER physicians backing?
The bills:
An Act Requiring Health Care Facilities to Develop & Implement Programs to Prevent Workplace Violence: Rep. Michael Moran, D-Boston. The measure most importantly would reclassify assault on a medical professional in the course of performing their duties as a felony. It would also require medical centers to write violence mitigation plans, develop an in-house crisis response team, support for victims of violence and regular reporting of incidents to administration, local police and district attorneys.
An Act Ensuring Access to Addiction Services: Rep. Ruth Balser, D-Newton. This measure reforms the Section 35 regulations that allow the involuntary commitment of alcohol-addicted people to treatment facilities. The regulation allows these men to be sent to carcel facilities if no other space is available. While earlier reforms prohibited women from being incarcerated, men are still allowed to be handcuffed and jailed for alcoholism. The measure would require expanded treatment capacity in settings administered by the departments of Public Health and Mental Health.
An Act Relative to Preventing Overdose Deaths and Increasing Access to Treatment: Rep. Dylan Fernandes, D-Falmouth, and Sen. Julian Cyr, D-Truro. The bill would establish a 10-year pilot program allowing municipalities to opt-in to locating an overdose prevention site within their community. Already established in countries worldwide and in New York City, the centers allow people with use disorders to use under direct medical supervision to prevent overdoses. The centers would also provide housing and food assistance, job training, referrals to treatment centers, drop-in services, medical interventions, drug testing and clean kits.
The Massachusetts College of Emergency Physicians, an advocacy organization dedicated to advancing excellence in emergency care, sponsored the legislative action day.
It conducts a twice-yearly survey to determine the extent of boarding in Massachusetts hospitals. The latest survey, conducted in January with a 72% response rate,k found that more than half the beds in emergency departments, 54%, were occupied by patients who had been seen, evaluated and were waiting for appropriate placements. Of those 171 patients were waiting for a bed in a behavioral health unit and 229 were awaiting transfer to an inpatient medical setting. The lack of beds is endemic across the state and throughout the country. In 1975 the U.S. had 1.5 million hospital beds; in 2022, that number was 917,000, with a population increase of 100 million people.
The most vulnerable patients are those with mental health issues, many of them children and teenagers; those with substance use disorders; the poor and elderly. Conditions that prompt them to seek emergency care can deteriorate as they are warehoused in hallways and waiting areas.
“It was 10 years ago, but I still remember it. A little girl was boarding at Boston Medical; she was maybe 10 or 12,” said Kathleen Coan, an emergency department doctor at Milford Regional Medical Center. It started to snow and would have been her first snowfall, but because she was a flight risk, the youngster wasn’t allowed to leave the emergency department to look out of a window and see the snow.
Her colleague Christopher DiTullio, a resident at UMass Memorial Medical Center, said many young people waiting for behavioral health beds spend 200, sometime 300 hours, waiting.
Hours waiting exacerbate illnesses, tempers
“It’s heartbreaking. They spend hours in what amounts to a dark closet playing video games, sleeping in chaos,” DiTullio said.
“Emergency department boarding is killing patients,” Kopp said. And it touches or has the potential to touch the lives of all Massachusetts residents. Overcrowding contributes to staff burnout, contributes to the increase in workplace violence against medical providers and is a factor in the exodus from the medical care field for doctors, nurses and support staff.
“People are leaving the medical profession in droves, and people in emergency departments are leaving even faster,” Kopp said. “It’s at the breaking point. People feel defeated.”
A different survey also conducted in January found that 91% of emergency physicians and 100% of nursing and support staff had been victims of violence. They had either suffered violence themselves, witnessed an incident or had a colleague who was victimized.
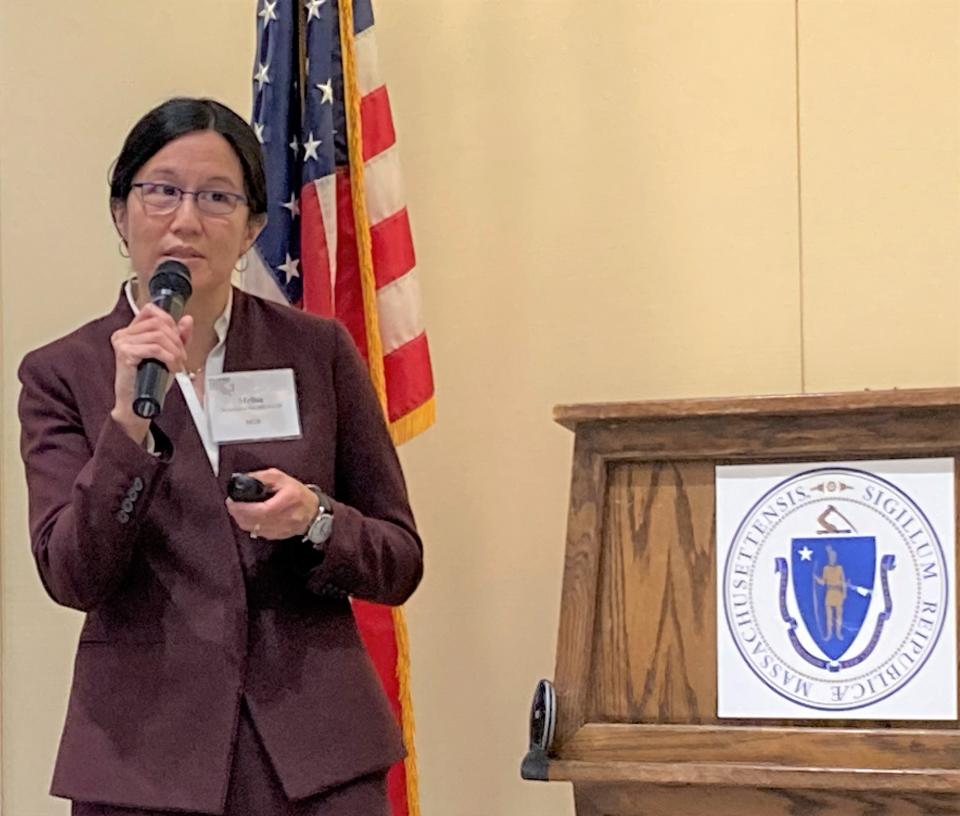
The bill supported by the advocacy group would prioritize the safety for all medical workers, said Dr. Melisa Lai Becker, an emergency physician at Massachusetts General Hospital. She noted that while many boarders are waiting for behavioral health beds, they are seldom the transgressors.
“It’s the patient in the next bed, or the visitor or family member of the patient in the next bed,” Lai Becker said. Even if police respond, officers cannot arrest and remove the offender if the attack is considered a misdemeanor. “The person is still there,” and the provider has to continue to treat them.
“Sometimes they taunt us or mutter under their breath that they’ll be coming back later with a gun,” Lai Becker said.
The widespread problem of violence in the workplace keeps Dr. Benjamin Milligan, head of emergency medicine at Cambridge Health Alliance, up at night.
“I fear getting a call in the night that one of my staff was assaulted,” Milligan said. “The bill is a tool to address the problem.”
Elevate assault on med staff to felony
Elevating assaults to felonies would extend protections to all medical workers, allied support staff, caseworkers, social workers, custodial and security staff. It would allow police to arrest the perpetrator and remove them from the situation.
The emergency docs back the idea of tackling the widespread opioid crisis differently, eschewing the “Just Say No” campaigns to establish harm reduction centers.

“In the last seven years, more than 2,000 people a year died of overdose deaths in Massachusetts. Those are our family, friends, neighbors, loved ones,” said Dr. Scott Weiner of Brigham & Women’s. Many emergency care centers already craft safe use kits that make clean syringes and needles, Naloxone and testing strips available.
The centers could save Boston medical centers $4 million a year in emergency service costs, factoring in the cost of everything related to an overdose emergency, from ambulances services to emergency medical treatment and the cost of dying.
“It’s evidence-based; it works,” Weiner said, citing statistics from the two centers that opened in New York City in November 2021. Since they opened through April, 5,004 users have accessed the centers with 135,000 experiences. Center staff have reversed 1,505 overdoses through the use of oxygen and supportive care.
“Do you know how many deaths they recorded? Zero,” Weiner said, adding the state cannot allow the cruel deaths to continue. “That’s the bottom line.”
This article originally appeared on Telegram & Gazette: Emergency physicians urge Mass. legislators to fix hospital overload

